Post written by Ahmir Ahmad, MRCP, from the Wolfson Unit for Endoscopy, St Mark’s Hospital, Harrow, London, UK.

Real-time optical diagnosis (OD) is now possible because of image-enhancing technologies offering the potential for huge cost and time savings associated with histopathology.
Despite several GI societies endorsing a “resect and discard” strategy for low-risk diminutive polyps, there has not been widespread adoption.
In the DISCARD3 study, we evaluated the OD learning curve and feasibility of a resect and discard strategy for ≤5-mm and <10-mm polyps in a bowel cancer screening setting. We assessed whether OD-histology surveillance interval concordance exceeds the 90% Preservation and Incorporation of Valuable Endoscopic Innovations threshold required for implementation of a resect and discard strategy. We also aimed to define a quality assurance process and assess patient acceptability.
DISCARD3 differs from earlier studies in that all 8 participating endoscopists were highly experienced, accredited bowel cancer screening colonoscopists. In addition, a robust quality assurance process was for the first time evaluated, and the patient perspective was explored with a survey and a focus group.
We also performed a detailed root-cause analysis of all cases of high-confidence OD error and evaluated the economic impact of a resect and discard strategy.
We found that the learning curve for OD in a bowel cancer screening setting varies between individual operators, with most able to perform consistently with an accuracy of ≥75%. A resect and discard strategy for high-confidence ≤5-mm polyp ODs is feasible and safe, with performance exceeding the 90% surveillance interval concordance threshold (with British Society of Gastroenterology [BSG], European Society of Gastrointestinal Endoscopy [ESGE] and U.S. Multi-Society Task Force guidelines) required for implementation in clinical practice.
For high-confidence OD of polyps <10 mm, the 90% surveillance interval threshold is exceeded for BSG and ESGE guidelines but not for U.S. guidelines. Most patients were satisfied with their procedures and supported an OD approach.
We also proposed a quality assurance process to support implementation of OD in clinical practice. A full economic analysis and detailed evaluation of the likely causes of OD error will be published separately.
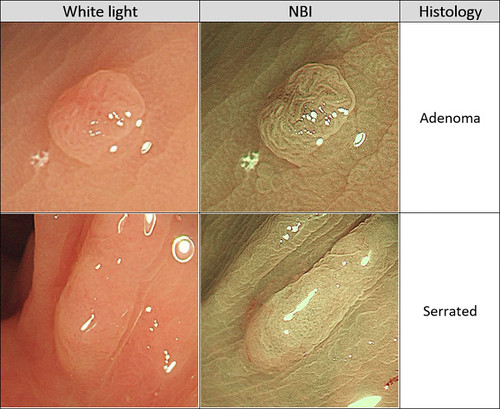 Optical diagnosis of adenomas and serrated lesions using narrow-band imaging. NBI, Narrow-band imaging.
Optical diagnosis of adenomas and serrated lesions using narrow-band imaging. NBI, Narrow-band imaging.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
