 Joan B. Gornals, MD, PhD, from the Endoscopy Unit, Department of Digestive Diseases, Hospital Universitari de Bellvitge-IDIBELL, in Barcelona, Spain discusses this New Methods article “EUS-guided methylene blue cholangiopancreatography for benign biliopancreatic diseases after failed ERCP.”
Joan B. Gornals, MD, PhD, from the Endoscopy Unit, Department of Digestive Diseases, Hospital Universitari de Bellvitge-IDIBELL, in Barcelona, Spain discusses this New Methods article “EUS-guided methylene blue cholangiopancreatography for benign biliopancreatic diseases after failed ERCP.”
The goal of this study was to describe and provide a new technique associated with interventional endoscopic ultrasound in cases of ERCP failed by biliopancreatic pathology. With the purpose of seeking to simplify the technique of EUS-biliary drainage intervention, and thereby improving our outcomes, procedure-time, and safety, we decided to replace the use of a guidewire (ie- Rendezvous) with the use of colorant (methylene blue, MB).
Our preliminary data suggest that EUS-guided cholangiopancreatography with MB seems to be feasible, effective, and safe in selected patients with benign biliopancreatic diseases in whom previous ERCP failed due to an undetectable papilla. This study is the first to specifically examine the efficacy and safety of MB injection for obtaining a CP and identification of the OP (orifice papilla) in benign biliopancreatic cases with previous failed ERCP due to unidentifiable OP.
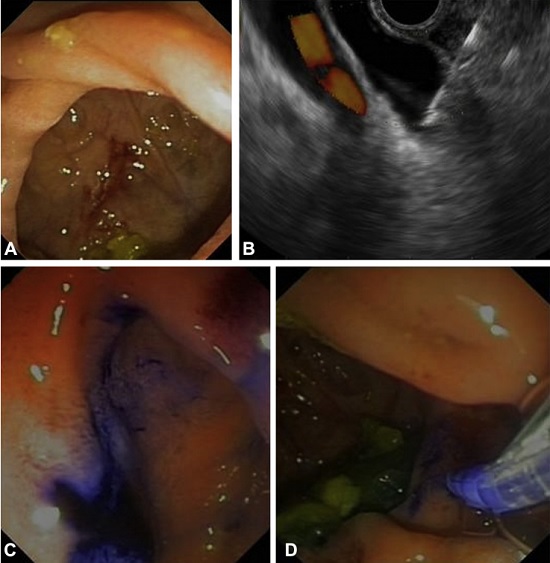
Figure 1. A, Endoscopic image of a periampullary diverticulum and undetectable orifice papilla. B, EUS-guided biliary access using a 22G needle. C, MB flow is identified coming from the major papilla orifice. D, Attempt at biliary cannulation with a sphincterotome (patient no. 5). MB, methylene blue.
In our study, all the patients had failed ERCP due to an unidentifiable or invisible papilla. Moreover, ductal access and papilla orifice detection were possible in all patients, and the overall rate of successful drainage was 91%. The most difficult part of the procedure was the papillary cannulation that requires good ERCP technique. But this is made easier by the ductogram map and the ‘pregnant’ effect of the papilla after EUS injection, as in a ‘parallel’ rendez-vous. No adverse events were related to the EUS-part of the intervention, and the only adverse event was attributed to a precut in an undetectable papilla case with altered anatomy.
Considerable experience in EUS-guided puncture is mandatory, especially if ducts are not dilated enough, and the optimal amount of MB is unknown. Finally, the operator needs to have sufficient experience in ERCP technique, including precut sphincterotomy. It is important to remark that our failure rate in native papilla ERCPs during the study period was 2.3%, similar to 1.7% reported recently by Holt et al (GIE 2015;81:104–110), that means a high quality of ERCP technique, and the scenario of an undetectable papilla is not common.
Find the article abstract here.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
