Post written by Rixta A.H. van Eijck van Heslinga, MD, and Leon M.G. Moons, MD, PhD, from the Department of Gastroenterology and Hepatology, University Medical Center Utrecht, Utrecht, The Netherlands.

The management of colorectal polyps with suspected deep submucosal invasive carcinoma (d-SMIC) remains a subject of ongoing debate. Optical assessment often overestimates the risk of d-SMIC, resulting in unnecessary surgeries for lesions that are, in fact, noninvasive or only superficially invasive.
Moreover, the presence of d-SMIC alone is associated with a relatively low risk of lymph node metastasis (2%-5%), raising questions about the clinical benefit of completion surgery, which carries a 1% to 1.7% perioperative mortality rate and does not eliminate the risk of distant metastasis. In response, the criteria for local excision of polyps suspected of d-SMIC have been broadened in The Netherlands, reflecting a patient-tailored, organ-preserving strategy in appropriately selected cases.
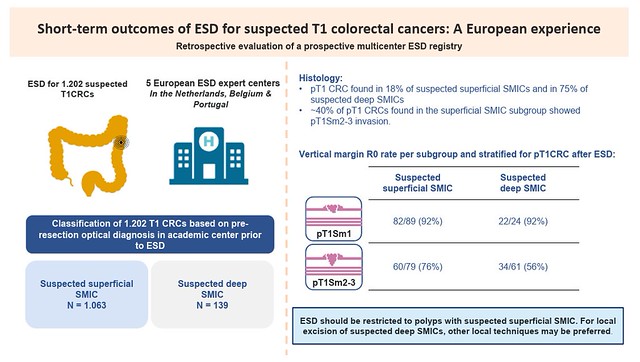
Endoscopic submucosal dissection (ESD) has been proposed as a staging procedure for polyps suspected of d-SMIC, but there is a lack of data on its effectiveness specifically in this subset of lesions. Most available studies focus on lesions suspected for superficial submucosal invasive carcinoma (s-SMIC), but few have explored ESD intentionally for d-SMIC. Our study aimed to fill this gap by evaluating the outcomes of an intentional ESD for suspected d-SMIC and comparing them with ESD for suspected s-SMIC.

This observational European multicenter study demonstrates that the outcomes of ESD for pT1 colorectal cancers (CRCs) are strongly influenced by the suspected depth of submucosal invasion. Although ESD achieves a high vertical margin radical resection rate for lesions suspected for s-SMIC, even for pT1Sm2-3 CRCs within this group, outcomes drop substantially for lesions suspected for d-SMIC. In the d-SMIC group, resections were more likely to fail, with a vertical margin radical resection rate of 56% (vs 76% in the s-SMIC group), highlighting the limitations of ESD in managing deeper invasive lesions.
Importantly, a significant proportion of lesions suspected for d-SMIC were found to contain high-grade dysplasia or pT1Sm1 CRC at histology (28%), underscoring the difficulty in accurately assessing submucosal invasion depth in routine clinical practice.
ESD remains highly effective for lesions suspected for s-SMIC, but this study shows that for lesions suspected for d-SMIC, alternative techniques, such as endoscopic full-thickness resection, intermuscular dissection, or laparoscopic wedge resection, may be preferred to optimize patient outcomes.
Our study emphasizes that ESD is an effective tool for pT1 CRCs, but its use should be restricted to polyps with suspected superficial submucosal invasion. For lesions suspected for deep submucosal invasion, alternative endoscopic techniques that may offer higher R0 resection rates should be considered. For local excision for suspected polyps, factors such as lesion size, malignant focus diameter, suspected invasion depth, and location in the colon or rectum should guide the choice of resection technique.
Graphical abstract
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
