Post written by Shruti Mony, MD, from the Department of Gastroenterology, Johns Hopkins University, Baltimore, Maryland, USA.

The focus of our study was to assess the recurrence patterns after endoscopic resection of nonampullary duodenal neuroendocrine tumors [DNETs]. Specifically, we wanted to identify the risk factors, effect of positive histologic margins, and optimal surveillance strategies including the duration of surveillance following endoscopic resection.
Duodenal neuroendocrine tumors account for <3% of intestinal carcinoids and typically follow an indolent course and carry a low metastatic potential. Their increasing incidence and prevalence have led to advances in curative endoscopic therapies. Endoscopic resection is performed for low-grade, superficial, and/or small (<1.0 cm) DNETs without lymphovascular invasion. (Endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), and endoscopic full thickness resection.)
Each bears its own advantages and disadvantages with the goal of achieving R0 resection. Thus, there exists a constant debate on the optimal treatment strategy and surveillance duration for DNETs, specifically in regard to risk factors for recurrence. Additionally, the duration and type of surveillance strategies in this population have not been well defined. Expert opinions from the European Neuroendocrine Tumor Society 2012 guidelines propose 6, 24, and 36 months of endoscopic follow-up with concurrent chromogranin A levels and CT or abdominal US which has not been validated by recent studies. We sought to answer these questions with our retrospective analysis in 3 different tertiary referral centers.
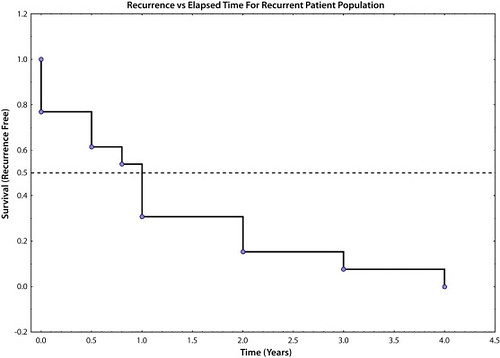
We found that of the 63 patients who underwent endoscopic resection of low-grade DNETs <1cm in size, the recurrence rate approached 20.6% with up to 69% of recurrences within the first year following resection. Independent of endoscopic resection technique, R1 or Rx margins were found to be a statistically significant risk factor for recurrence in this population (P = .048). The mean surveillance time for all DNETs was 2.8 ± 2.6 years. We noted that more frequent and earlier surveillance after resection (within 1-3 year period) was preferred in order to capture recurrences. This was contrary to that recommended by European Neuroendocrine Tumor Society guidelines. Additionally, since no recurrences occurred in our cohort after 4 years, it is likely safe to reduce surveillance frequency, questioning the need for continued close surveillance, especially in those with negative margins.
As advances to endoscopic resection continues, further studies with a larger sample size are needed to evaluate the risk of recurrence after endoscopic resection in DNETs between 1-2 cm as well as determine the sequela of a delay in recurrent DNET management.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.