Post written by Shinji Tanaka, MD, PhD, FASGE, FACG, from the Endoscopy and Medicine, Graduate School of Biomedical & Health Sciences, Hiroshima University.
JNET classification is composed of four types (Type 1, 2A, 2B, and 3) with two NBI magnifying findings, surface pattern and vessel pattern. Type 1, 2A, 2B, and 3 are supposed to indicate their respective histology. Type 1represents hyperplastic polyp (HP) and sessile serrated polyp (SSP). Type 2A represents low-grade dysplasia (LGD), such as tubular adenoma/tubulovillous adenoma. Type 2B represents high-grade dysplasia (HGD) and superficial submucosal invasive carcinoma (SM-s carcinoma). Type 3 represents deep submucosal invasive carcinoma (SM-d carcinoma). As we reported before, Type 1, 2A, and 3 are highly reliable indicators for their respective most likely histology, with significant qualitative and quantitative accuracy. On the other hand, the ability of Type 2B to indicate HGD and SM-s carcinoma is comparatively weaker than other three types because it contains lesions with various histology ranging from LGD to SM-d carcinoma. This study aimed to determine whether or not subtyping of Type 2B improves diagnostic performance.
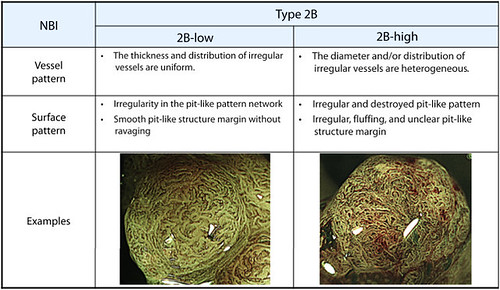
Figure 2. Subtyping of Japan NBI Expert Team Type 2B. NBI, Narrow-band imaging.
We subclassified the Type 2B lesions as 2B-low and 2B-high based on the level of irregularity in vessel and surface patterns. Type 2B-low lesions exhibited uniform thickness and distribution of irregular vessels, an irregularity in network of the pit-like pattern, and a smooth margin of the pit-like pattern without ravage. Type 2B-high lesions exhibited heterogeneous diameters and/or distributions of irregular vessels, an irregular and destroyed pit-like pattern, and irregular, fluffing, unclear margin of the pit-like pattern (Fig. 2).
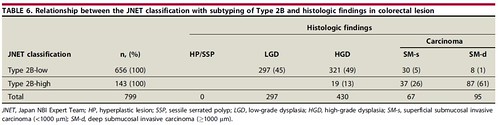
For JNET Type 2B subtyping, about 80% of Type 2B lesions were classified as Type 2B-low. Further, most of all Type 2B-low lesions were LGD, HGD, and SM-s carcinoma (Table 6). Since almost all Type 2B-low lesions were LGD, HGD, and SM-s carcinoma, Type 2B-low can be regarded as a reliable indicator for endoscopic resection among the various types of histology in Type 2B. On the other hand, 61% of Type 2B-high lesions were SM-d carcinoma, which requires surgery, while the remaining lesions were HGD and SM-s carcinoma. This suggested that Type 2B-high is not a reliable indicator for surgery. Thus, for Type 2B-low lesions, which comprise about 80% of Type 2B lesions, endoscopic treatment can be a first choice in the therapeutic strategy process. As lesions with Type 2B-high alone cannot be determined as SM-d carcinoma, further examination is necessary to differentiate HGD and SM-s carcinoma from SM-d carcinoma to avoid unnecessary surgery. To determine the appropriate treatment method (endoscopic resection or surgery) for Type 2B-high lesions, pit pattern diagnosis using chromoagents or endoscopic ultrasonography (EUS) is necessary to diagnose the correct invasion depth.
Thus, the Type 2B subtyping may improve the diagnostic performance of the JNET classification and contribute to daily colonoscopic practice.
Please note: The authors emphasize that this trial using JNET classification is a private pilot study of Hiroshima University. This Type 2B subclassification is not the consensus of JNET. At present, “JNET classification” is ongoing to be validated and refined by all members of JNET.
Find the article abstract here.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
