 Editor-in-Chief, Dr. Michael Wallace, highlights this article from the July issue “Colorectal cancer screening: Recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer” by Douglas K. Rex, MD, et al.
Editor-in-Chief, Dr. Michael Wallace, highlights this article from the July issue “Colorectal cancer screening: Recommendations for physicians and patients from the U.S. Multi-Society Task Force on Colorectal Cancer” by Douglas K. Rex, MD, et al.
Colorectal cancer screening is likely the single most common activity performed by gastroenterologists in the United States. Every few years, the U.S. Multi-Society Task Force, led by Doug Rex, updates national guidelines on how we should perform CRC screening. GIE is proud to co-publish this landmark guideline in partnership with The American Journal of Gastroenterology and Gastroenterology.
All physicians who perform or order CRC screenings need to be up-to-date on the most recent recommendations. Here a few take-home points from the article.
- It is recommended that clinicians offer CRC screening beginning at age 50 (strong recommendation, high-quality evidence).
- It is suggested that sequential offers of screening tests, multiple screening options, and risk-stratified screening are all reasonable approaches.
- Recommended tests are divided into 3 tiers:
- Tier 1: (top recommendation) includes colonoscopy or annual FIT testing.
- Tier 2: CT colonography every 2 years, FIT-Fecal DNA every 3 years, or Flexible sigmoidoscopy every 5 to 10 years.
- Tier 3: Capsule colonoscopy every 5 years.
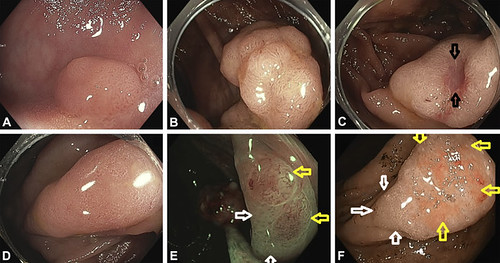
Figure 1. Enter aEndoscopic photographs of conventional adenomas and sessile serrated polyps. A, Small (8-mm diameter) conventional adenoma. The red lines are surface blood vessels. B, A portion of a 40 mm advanced conventional adenoma; one of the targets of all screening tests. The prominent blood vessel pattern is again visible. C, A conventional adenoma with a focus of invasive cancer. The prominent blood vessel pattern of a conventional adenoma visible over the lesion except in the ulcerated area. The cancer is located at the ulcer (arrows) D, A sessile serrated polyp without cytologic dysplasia. Note the absence of blood vessels on the surface. E, A sessile serrated polyp (visualized in narrow-band imaging) with multiple foci of cytologic dysplasia (yellow arrows). The dysplastic areas have the blood vessel pattern (and the histologic features) of an adenoma. The white arrows point to non-dysplastic portions of this sessile serrated polyp. F, A sessile serrated polyp with invasive cancer; white arrows designate the residual sessile serrated polyp, whereas yellow arrows indicate the ulcerated malignant portion of the lesion caption
Read the article abstract here.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
