Post written by Andrew Canakis, DO, from the Division of Gastroenterology and Hepatology, TidalHealth Peninsula Regional Medical Center, Salisbury, Maryland, USA.

The aim of this study was to investigate mid-term clinical outcomes after EUS-guided gallbladder drainage (EUS-GBD), with a focus on clinical success and the rate of recurrent cholecystitis.
Although a multitude of studies have demonstrated the high technical success of this transmural drainage approach, less is known about durability once patients leave the index hospitalization. As EUS-GBD becomes more widely adopted, procedure-related clinical metrics (ie, stent patency, need for reintervention, and readmission rates) are increasingly important to define.
This is particularly relevant as more institutions incorporate EUS-GBD into treatment algorithms for acute cholecystitis in high-risk surgical candidates, where long-term drainage performance directly informs patient selection, follow-up strategy, and expectations for recurrence. To our knowledge, this is the first meta-analysis to specifically explore clinical outcomes (with a follow-up of at least 1 year) for EUS-GBD in patients with acute cholecystitis.
Our study supports the use of EUS-GBD as a technically reliable and clinically effective management option for acute cholecystitis. We found that the technical and clinical success rates were 95.8% and 94.3%, respectively. This shows that despite varying techniques, stent sizes, and postprocedural follow-up protocols, the overcall clinical success rate was high across all geographic study locations and time periods.
Reintervention was uncommon (6%) and late recurrence of cholecystitis at 1 year or longer was low (4.2%), supporting sustained drainage and stent patency for most patients. Finally, the overall low adverse event rate highlights a key advantage of EUS-GBD: it offers definitive, minimally invasive therapy for patients in whom operative management carries prohibitive risk.
Moving forward, comparing different stent-related procedure and management options can help further refine clinical outcomes. The procedure is not standardized, and there is notable heterogeneity in the transmural drainage site (stomach versus duodenum), stent size, use of plastic stents, and postprocedural stent management (leaving the lumen-apposing metal stent in place or exchanging for 2 plastic pigtail stents).
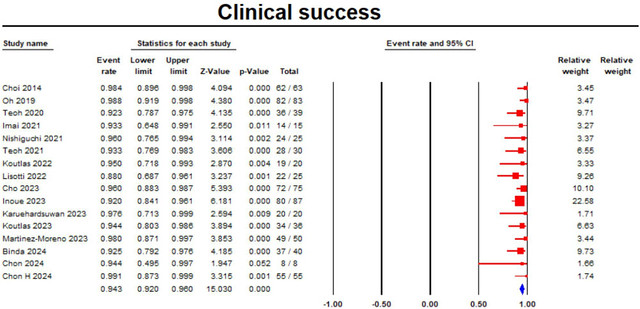
The pooled rate of clinical success.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
