Post written by Giuseppe Vanella, MD, PhD, from San Raffaele Hospital, Vita-Salute San Raffaele University, Milan, Italy.

When dealing with symptomatic or infected peripancreatic fluid collections (PFCs), EUS-guided drainage has become the standard of care. In about one-half of cases, drainage alone will be enough to solve the issue. Yet, a fraction of patients will require further interventions, such as direct endoscopic necrosectomy, additional drainage tracts, or percutaneous/surgical rescue, following the so-called “step-up approach.”
Until now, a simple, reliable, and broadly applicable predictive tool to identify these high-risk patients was missing. Most available evidence came from retrospective studies focusing only on walled-off necrosis and the use of lumen-apposing metal stents, often overlooking other types of collections and alternative stenting strategies.
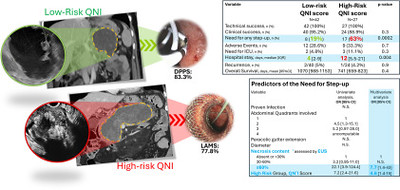
Our study stemmed from a prospective registry enrolling all consecutive patients requiring EUS-guided PFC drainage in a tertiary referral center to evaluate independent predictors of step-up to additional procedures. We assessed the role of factors previously explored in retrospective literature, but we especially focused on the recently available Quadrant-Necrosis-Infection (QNI) score, developed by colleagues at Mayo Clinic.1 Incorporating necrosis extent, number of abdominal quadrants involved, and presence of infection, the score stratifies PFCs into low- and high-risk categories. However, it had yet to be prospectively validated.
We prospectively enrolled 70 consecutive patients with PFCs, including walled-off necrosis, pseudocysts, and postsurgical collections. About 40% were treated with lumen-apposing metal stents, and the rest with double-pigtail plastic stents. The overall treatment results were encouraging: technical success was 100% and clinical success 93%, with negligible recurrence. However, 36% of patients required step-up procedures (mostly necrosectomy), as drainage alone was insufficient.
Two factors emerged as independent predictors for this more-complex treatment course: the classification in the QNI high-risk group and (independently) necrosis extent greater than 60%. Interestingly, collection size alone and microbiologically proven infection were not predictive.
We also compared necrosis assessment by radiology (CT/magnetic resonance imaging) and EUS. Although interobserver agreement within each modality was excellent, between-modalities agreement was low, as EUS tended to identify more-extensive necrosis than radiology and better predicted a more-complex disease course. This supports the role of real-time EUS assessment in guiding decisions such as stent type, timing of necrosectomy, or early adoption of additional step-up procedures.
Looking ahead, our findings confirm the prognostic value of the QNI score and suggest greater emphasis on necrosis extent (≥60%). Larger multicenter studies will be key to evaluate the real-world clinical impact of this stratification, potentially informing more-personalized strategies, guiding decisions on centralization to high-volume centers, influencing the hospitalization regimen, anticipating longer hospital stay, and prompting earlier access to secondary interventions when needed.
Graphical abstract
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
- Baroud S, Chandrasekhara V, Storm, AC, et al. Novel classification system for walled-off necrosis: a step toward standardized nomenclature and risk-stratification framework. Gastrointest Endosc 2023;97:300-8. ↩︎
