Post written by Ahmad Abdulraheem, MD, and Angela Koomson, MD, from the Department of Medicine, MedStar Georgetown Washington Hospital Center, and Abdalla Khouqeer, MD, Ahmad Al-Dwairy, MD, and Walid Chalhoub, MD, from the Gastroenterology Section, Department of Medicine, MedStar Georgetown University Hospital, Washington, District of Columbia, USA.

The video describes a case of severe bile duct injury managed solely with ERCP. The patient presented with acute cholecystitis due to choledocholithiasis and initially underwent ERCP with placement of a plastic stent.
A day later, laparoscopic cholecystectomy was performed and complicated by a severe Strasberg type D bile duct injury, an uncommon form of injury. After multidisciplinary discussion between the hepatobiliary team and advanced endoscopists, a second ERCP was performed, and the patient was successfully treated with ERCP alone by exchanging the plastic stent.
Traditionally, management of this injury involves hepatobiliary surgery. Follow-up imaging confirmed resolution of the bile leak.
This article suggests that minimally invasive endoscopic techniques may be promising in certain cases of advanced bile duct injuries, offering a potential alternative to traditional hepatobiliary surgery, although this approach is still under investigation.
Endoscopists can consider endoscopic management for bile duct injuries in carefully selected cases, taking into account factors such as the extent of transection, patient stability, timing of intervention, imaging findings, and intraoperative assessment of biliary anatomy. Reporting these cases will help build a larger sample size to evaluate the efficacy of ERCP versus surgery, particularly regarding postprocedural adverse events such as strictures.
Multidisciplinary team discussions between advanced endoscopists and hepatobiliary surgeons should always be conducted to determine the optimal management approach.
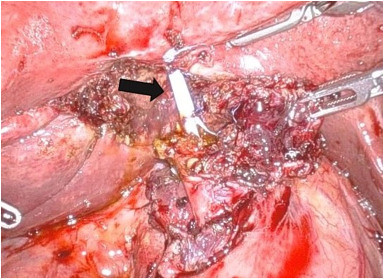
Laparoscopic cholecystectomy showing a common bile duct injury with an exposed plastic stent (black arrow).
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
