Post written by Shunya Takayanagi, MD, from the Department of Gastroenterology, NTT Medical Center Tokyo, Tokyo, Japan.

In this study, we reported the use of EUS-guided nasocavitary catheter drainage to treat an intra-abdominal abscess caused by delayed perforation after gastric endoscopic submucosal dissection (ESD). A 78-year-old man with early gastric cancer in the lesser curvature of the stomach underwent ESD without intraprocedural complications. On postoperative day (POD) 5, he was diagnosed with an intra-abdominal abscess caused by delayed perforation.
However, the fistula was closed endoscopically and managed conservatively, which was not effective. EUS-guided drainage was performed because it was a less invasive treatment. On POD 34, a follow-up CT revealed the complete resolution of the abscess, and the tube was removed.
Delayed perforation after gastric ESD is still a serious complication often requiring emergency surgery. However, with the recent advancement of endoscopic techniques and the development of devices, there are more cases in which the fistula can be closed and treated conservatively without emergency surgery. In these cases, conversely, the closure of the fistula seems to prevent spontaneous drainage and worsen the abscess.
Generally, antibiotics poorly penetrate an established abscess; hence, surgery and percutaneous drainage are often required. Percutaneous drainage is often used as a first-line treatment for intra-abdominal abscesses and is a less invasive treatment than surgical drainage. Because the intra-abdominal abscesses caused by the perforation after gastric ESD are thought to be located adjacent to the gastric wall, drainage via the gastric wall is more effective and direct than percutaneous drainage.
During the procedure, a 19-gauge needle (EZ Shot 3 Plus; Olympus Medical, Tokyo, Japan) is inserted into the abscess adjacent to the gastric wall under continuous EUS and fluoroscopic guidance, and a 0.025-inch guidewire (Visiglide2; Olympus Medical) is inserted through the needle, followed by the insertion of a 6F nasobiliary drainage tube (SilkyPass; Boston Scientific, Marlborough, Mass, USA) via surrounding normal mucosa into the cavity.
In conclusion, EUS-guided drainage of an abscess occurring after ESD is a minimally invasive treatment that can be used immediately in clinical practice.
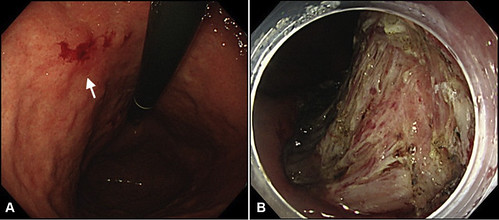 Endoscopic findings. A, The lesion (white arrow) was located in the lesser curvature of the stomach. B, Endoscopic submucosal dissection was performed without intraoperative perforation.
Endoscopic findings. A, The lesion (white arrow) was located in the lesser curvature of the stomach. B, Endoscopic submucosal dissection was performed without intraoperative perforation.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
