Post written by Brett J. Hoskins, DO, from the Division of Pediatric Gastroenterology, Hepatology, and Nutrition, Department of Pediatrics, Indiana University School of Medicine, Riley Hospital for Children at IU Health, Indianapolis, Indiana, USA.

This video demonstrates ischemic polypectomy during balloon-assisted enteroscopy in a 12-year-old girl with Peutz-Jeghers syndrome and chronic iron deficiency anemia. Seven pedunculated small-bowel polyps were treated using a detachable snare to mechanically strangulate the stalk and induce autoamputation, without the use of electrocautery.
The video features 3 representative cases, including a real-world example of device malfunction requiring repeat snare placement. All polyps were successfully treated without bleeding or perforation, and the patient experienced meaningful clinical improvement, with hemoglobin rising from 9.1 to 12.4 g/dL at follow-up.
Small-bowel polyps are common in pediatric patients with Peutz-Jeghers syndrome and represent a major source of morbidity, including bleeding, anemia, and intussusception. Many children ultimately require bowel surgery for obstructive adverse events, making the availability of therapeutic deep enteroscopy an important tool for reducing cumulative surgical burden. Pediatric small-bowel polypectomy presents unique technical and safety challenges because of thinner bowel walls, narrower lumens, and higher risk of deep thermal injury associated with electrocautery in this setting.
Although ischemic polypectomy has been described in adults, visual documentation in children has been extremely limited. To our knowledge, this represents the first published video demonstration of this technique in a pediatric patient. We felt it was important to provide practical, real-world guidance for managing high-risk small-bowel polyps in this vulnerable population.
This case highlights several technical pearls, including careful positioning of the detachable snare at the stalk base, slow tightening with visual confirmation of sustained ischemic color change, and readiness to reattempt deployment if device malfunction occurs. Importantly, ischemic polypectomy allows treatment without electrocautery, which may reduce the risk of transmural thermal injury in the thin-walled pediatric small bowel. When combined with balloon-assisted enteroscopy, this approach offers a valuable option for safely managing multiple pedunculated lesions while potentially decreasing bleeding risk, perforation risk, and need for surgical intervention.
As pediatric deep enteroscopy becomes more widely available, sharing reproducible therapeutic techniques is essential. We hope this video helps expand the procedural toolbox for pediatric endoscopists caring for children with hereditary polyposis syndromes and encourages thoughtful adoption of nonthermal resection strategies in appropriate patients.
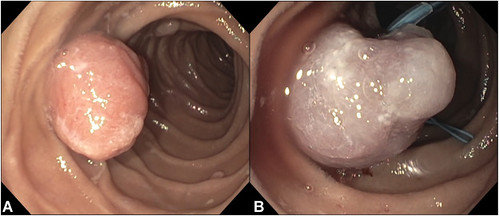
Endoscopic images from ischemic polypectomy in a 12-year-old girl with Peutz-Jeghers syndrome: (A) 20-mm pedunculated jejunal polyp prior to intervention; (B) same polyp after deployment of a detachable snare on the stalk, demonstrating dusky discoloration consistent with vascular strangulation and early ischemia.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
