Post written by Aman Yadav, MD, and Alexander Huelsen, MD, from Department of Gastroenterology & Digestive Health, Gold Coast University Hospital, Southport, Australia.

In our video, we demonstrate a simple and reproducible gastroscope-assisted method to examine the oral cavity and nasopharynx during routine EGD. With the use of a standard diagnostic gastroscope equipped with a distal cap, the oral cavity is assessed presedation through 4 standardized positions—tongue down, right, left, and up—allowing stable, high-resolution visualization of the tongue, buccal mucosa, palate, and uvula. The nasopharynx is evaluated upon withdrawal of the gastroscope in the pharynx in sedated patients by retroflexing the cap-assisted gastroscope.
Each examination takes less than 20 seconds and requires no additional equipment. The video focuses on presenting normal anatomy and the ease with which these often-overlooked areas can be incorporated into routine practice.

We felt it was important to highlight this technique because the oral cavity and nasopharynx remain routinely underexamined during EGD, despite being part of the same anatomical pathway. These areas can harbor mucosal abnormalities, including early neoplastic changes, that may go undetected without deliberate inspection.
To our knowledge, there is limited standardization on how GI endoscopists should approach these regions, which can contribute to variability in practice. By showcasing a simple, structured method using equipment already available in every endoscopy unit, we hope to encourage wider awareness and opportunistic screening, particularly in high-risk populations. The video also provides a practical anatomical reference for trainees who may be less familiar with structures above the upper esophageal sphincter.
Endoscopists can learn that brief systematic assessment of the oral cavity and nasopharynx is both feasible and highly informative when performed with a cap-assisted gastroscope. The 4-position oral cavity technique provides stable views of commonly missed structures, allowing abnormalities such as erosions, plaques, or leukoplakia to be recognized and appropriately referred. The nasopharynx maneuver demonstrates that retroflexion with a distal cap is safe and yields excellent visualization in the majority of patients, without prolonging procedure time. Our experience reinforces that GI endoscopists can incorporate these steps with a minimal learning curve. This approach enhances diagnostic thoroughness and adds educational value for trainees seeking to broaden their anatomical familiarity.
These techniques integrate seamlessly into existing EGD workflows and align with the broader movement toward comprehensive upper aerodigestive assessment. Although GI endoscopists may feel less confident above the upper esophageal sphincter, clear documentation and referral pathways, particularly to ear-nose-throat colleagues, help ensure safe and appropriate management of any abnormalities encountered. The low cost and universal availability of distal caps make the method accessible across diverse practice settings.
We are planning prospective work to assess diagnostic yield, catalogue typical pathologies, and evaluate uptake among trainees. We hope this standardized approach encourages other groups to explore expanded visualization during EGD and contributes to earlier recognition of mucosal disease in these often-overlooked regions.
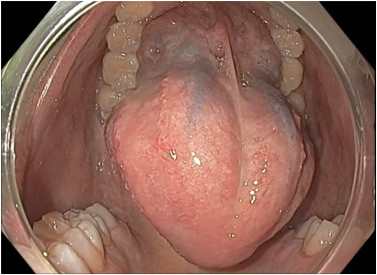
Fourth standard image of the oral cavity with tongue up.
Read the full article online.
The information presented in Endoscopedia reflects the opinions of the authors and does not represent the position of the American Society for Gastrointestinal Endoscopy (ASGE). ASGE expressly disclaims any warranties or guarantees, expressed or implied, and is not liable for damages of any kind in connection with the material, information, or procedures set forth.
